Can I draw blood from a PIVC?
)
Drawing blood from a cannula is a routine practice in some clinical environments. But is this best practice or will the blood become too haemolysed to provide accurate results?
Drawing blood from a peripheral intravenous catheter/cannula (PIVC) is a routine practice in clinical environments such as the emergency department, rationalised as one less invasive test that a patient is subjected to. A PIVC should never be inserted just to draw blood or 'just in case' it's needed later. Up to 50% of PIVCs inserted in the emergency department are never used! And this increases the risk of bloodstream infections.
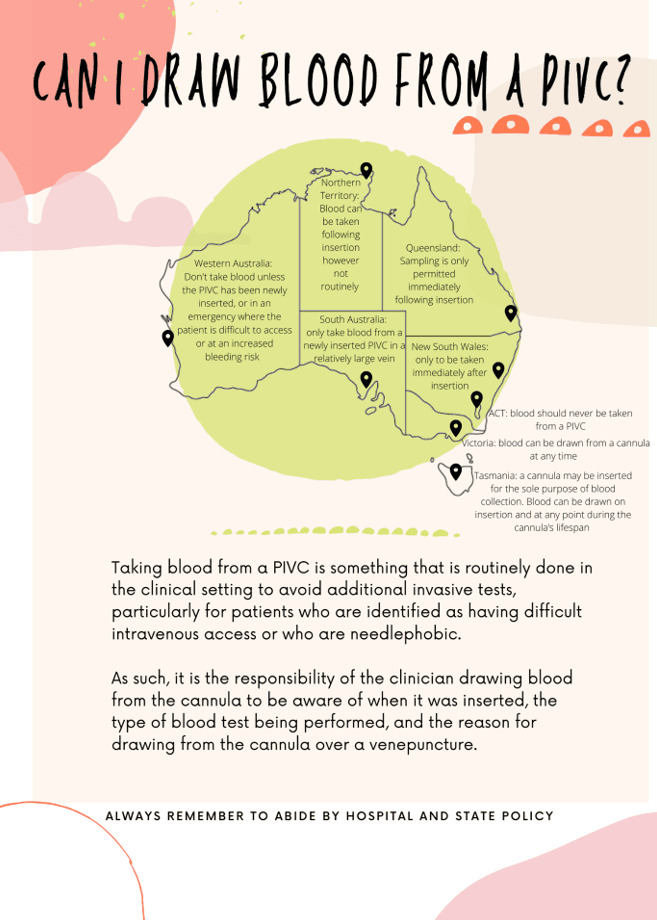
There is a distinct lack of knowledge surrounding the appropriate timing and manner to collect blood from a cannula (Jacob et al, 2021). Accessing information on blood-drawing policy can be tricky, as there are significant nuances between Australian states and territories. The poster is a summary of recommendations across Australia. The consensus is that immediately following insertion, blood can be drawn from a PIVC, however in the ACT this is forbidden due to the risk of haemolysis. As such, it is the clinician's responsibility to familiarise themselves with state and institution policy in order to provide the safest care, which can be difficult as policies are not always easily accessible or up to date.
Defined as the destruction of erythrocytes (red blood cells), haemolysis can occur physiologically (such as in a mismatched blood transfusion), or externally as a result of incorrect collection or storage of blood specimens (Law & Martin, 2020). Although recent evidence suggests no difference between rates of haemolysis in cannula-drawn blood versus venepuncture-drawn blood, ongoing divergence in state and local policy means that it is very difficult for clinicians to decipher what is appropriate, with many states and territories failing to adapt to nuances in evidence-based practice (Jacob et al., 2021).
At all times, keep in mind what is the best thing for the patient. For instance, if the patient is very unwell, one must ask whether they have the time to wait for the results of peripherally drawn bloods only to return an inaccurate reading and have to retake venous blood. Similarly, if a patient coming into the emergency department is extremely needlephobic, is it in their best interest to avoid another invasive test that can bring on significant anxiety?
As with most decisions in the clinical environment, the clinician needs to make an educated choice in conjunction with state and institution policy.
References
Coventry, L., Jacob, A., Davies, H., Stoneman, L., Keogh, S., & Jacob, E. (2019). Drawing blood from peripheral intravenous cannula compared with venepuncture: A systematic review and meta-analysis. Journal of Advanced Nursing, 75(11), 2313-2339.
Davies, H., Coventry, L., Jacob, A., Stoneman, L., & Jacob, E. (2020). Blood sampling through peripheral intravenous cannulas: a look at current practice in Australia. Collegian, 27(2), 219-225.
Gledstone-Brown L, McHugh D. Review article: Idle 'just-in-case' peripheral intravenous cannulas in the emergency department: Is something wrong? Emerg Med Australas 2018;30(3):309-326
Jacob, E., Jacob, A., Davies, H., Jacob, D., Jenkins, M., Husain, M., & Coventry, L. (2021). The impact of blood sampling technique, including the use of peripheral intravenous cannula, on haemolysis rates: A cohort study. Journal of Clinical Nursing, 30(13-14), 1916-1926.
Jacob, E., Jacob, A., Davies, H., Stoneman, L., & Coventry, L. (2021). Peripheral intravenous cannulas for blood drawing: Nurses' views through content analysis. Collegian, 75(11), 2313-2339.
Law, J., & Martin, E. (2020). Concise Medical Dictionary.
Australian guidelines (provided only for those with online links)
Australian Commission on Safety and Quality in Health Care (2021). Management of Peripheral Intravenous Catheters Clinical Care Standard. Sydney: ACSQHC; 2021. https://www.safetyandquality.gov.au/standards/clinical-care-standards/management-peripheral-intravenous-catheters-clinical-care-standard
ACT Health (2019). Peripheral Intravenous Cannula (PIVC), Adults and Children (Not neonates). https://www.health.act.gov.au/sites/default/files/2019-02/Peripheral%20Intravenous%20Cannula2C%20Adults%20and%20Children%20%28Not%20neonates%20.docx
National Health and Medical Research Council (2019). Australian Guidelines for the Prevention and Control of Infection in Healthcare. Canberra: Commonwealth of Australia. www.nhmrc.gov.au/health-advice/public-health/preventing-infection
NSW Health. (2019). Intravascular Access Devices (IVAD) - Infection Prevention and Control. https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/PD2019_040.pdf
Queensland Health (2019). Recommendation for the prevention or infection in intra-vascular devices. https://www.health.qld.gov.au/__data/assets/pdf_file/0025/932830/intra-vascular-devices.PDF
SA Health. (2020). Peripheral Intravenous Catheter (PIVC) Infection Prevention Clinical Directive. https://www.sahealth.as.gov.au/was/wcm/connect/b8b0b71d-899e-42aa-ac3bxca37d905f9a8/Clinical_Directive_PIVC_Infection_Prevention_v1.0_22.11.2019.PDF?MOD=AJPERES
WA Department of Health. (2017). Insertion and Management of Peripheral Intravenous Cannulae in Western Australian Healthcare Facilities Policy. https://ww2.health.wa.gov.au/~/media/Files/Corporate/Policy%20Frameworks/Public%20Health/Policy/Insertion%20and%20Management%20of%20Peripheral%20Intravenous%20Cannulae/MP38-Insertion-and-Management-of-Peripheral-Intravenous-Cannulae.pdf
| Tags:peripheral intravenous catheterblood samplingvenepuncture |








