Central line bloodstream infections: CLABSI or CRBSI?
)
Central venous access devices (CVADs) are an essential component of contemporary medical care, allowing for incompatible medications to be administered simultaneously and reduce the need for peripheral vascular access, particularly for critically ill or oncology patients.1
However, CVADs can entail significant risk. Bloodstream infection is the most detrimental consequence of inadequate CVAD management, presenting a significant burden to the patient, staff and economy of a hospital, especially as 65%–70% of cases are preventable.2 CVADs account for up to 70% of hospital-acquired bloodstream infections, which if left untreated, can lead to sepsis.3,4
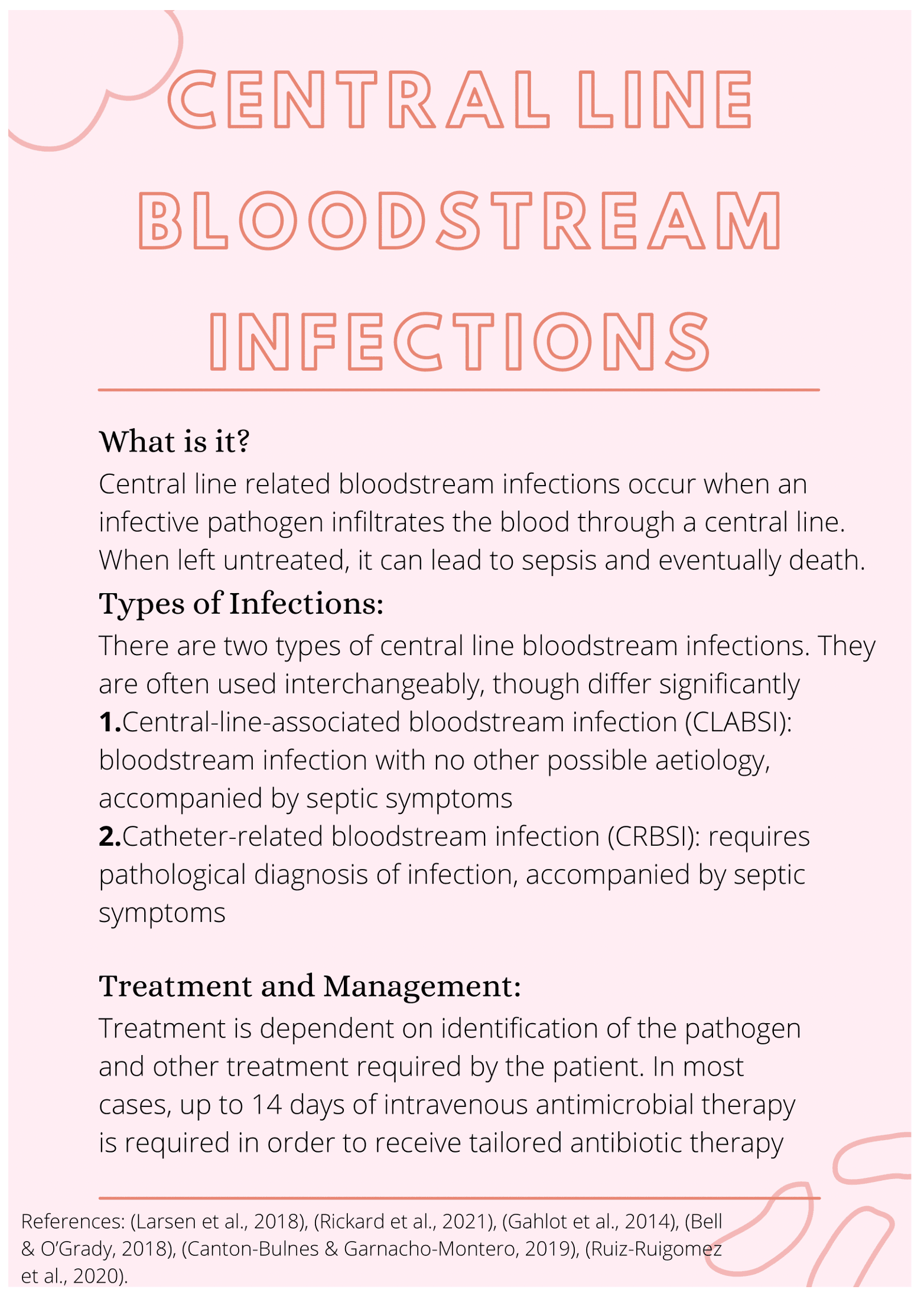
Two ways of identifying a bloodstream infection in a patient with a central line are commonly used in the clinical setting. Although often used interchangeably, these terms are independent from each other5,6.
Central-line-associated bloodstream infection (CLABSI) is defined as a bloodstream infection in a patient with a central line in situ or removed in the last 48 hours, with no other obvious cause of infection7.
Catheter-related bloodstream infection (CRBSI) requires a pathological diagnosis through positive blood cultures7.
Both are managed according to the causative pathogen, however as CRBSI requires a definitive diagnosis potentially not available at all hospitals, CLABSI is the more common diagnosis.7
Without prompt treatment, bloodstream infection can progress rapidly to septicaemia, multi-organ failure and death8. Therefore, broad-spectrum intravenous antibiotics should be commenced as soon as BSI is suspected, even before confirmation of the bacteria.9 Once the invading pathogen is confirmed, treatment can be tailored to more specific antimicrobial therapy, and will likely continue for up to 14 days, meaning a prolonged hospital stay and costs to the healthcare sector.8
References
1. Ho C, Spry C. Central venous access devices (CVADs) and peripherally inserted central catheters (PICCs) for adult and pediatric patients: A review of clinical effectiveness and safety. Ottawa: Canadian Agency for Drugs and Technologies in Health; 2017.
2. Larsen E, Gavin N, Marsh N, Rickard C, Runnegar N, Webster J. A systematic review of central-line-associated bloodstream infection (CLABSI) diagnostic reliability and error. Infection Control & Hospital Epidemiology 2019;40(10):1100-6.
3. Smyth ET, McIlvenny G, Enstone JE, Emmerson AM, Humphreys H, Fitzpatrick F, et al. Four country healthcare associated infection prevalence survey 2006: overview of the results. J Hosp Infect. 2008;69(3):230-48.
4. Gahlot R, Nigam C, Vikas K, Yadav G, Anupurba S. Catheter-related bloodstream infections. International Journal of Critical Illness and Injury Science 2014;4(2):162-7.
5. Bell T, O'Grady NP. Prevention of central line-associated bloodstream infections. Infect Dis Clin North Am. 2017;31(3):551-9.
6. Centers for Disease Control and Prevention. Guidelines for the Prevention of Intravascular Catheter-Related Infections; 2011; Available from: https://www.cdc.gov/infectioncontrol/guidelines/bsi/background/terminology.html.
7. Bell T, O’Grady N. Prevention of central line-associated bloodstream infections Infectious Disease Clinics of North America 2018;31(3):551-9.
8. Kornbau C, Lee K, Hughes G, Fistenberg M. Central line complications. International Journal of Critical Illness and Injury Science 2015;5(3):170-8.
9. Canton-Bulnes M, Garnacho-Montero J. Practical approach to the management of catheter-related bloodstream infection. Official Journal of the Spanish Society of Chemotherapy 2019;32(2):38-41.
Other
Rickard C, Marsh N, Larsen E, McGrail M, Graves N, Runnegar N, et al. Effect of infusion set replacement intervals on catheter-related bloodstream infections (RSVP): a randomised controlled, equivalence (central venous access device) - non-inferiority (peripherally arterial catheter) trial The Lancet 2021;397(10283):1447-58.
Ruiz-Ruigomez M, Fernandez-Ruiz M, San-Juan R, Lopez-Medrano F, Orellana M, Corbella L, et al. Impact of duration of antibiotic therapy in central venous catheter-related bloodstream infection due to Gram-negative bacilli. Journal of Antimicrobial Therapy 2020;75(10):3049-55.
| Tags:central vascular access devicescatheter-associated bloodstream infection |








